Implementation
The MES introduces medical examiner scrutiny to the completion of the Medical Certificate of Cause of Death (MCCD) for non-coronial deaths. The MES moved to a statutory footing on 9 September 2024.
The purpose of this guidance is to remind GPs of the role and function of the medical examiners, together with associated practical implications.
Post-implementation feedback from medical examiners
Updated August 2025
Londonwide LMCs had a recent meeting with our London regional senior medical examiner (ME) colleagues to find out on how the first year of the MES to a statutory footing had gone. Key points included:
- GP practices have responded well to the statutory move and have co-operated positively with MES offices.
- The medical examiner offices have in general terms been grateful for the way in which GPs and their practices have adapted to the new procedures.
- Differences remain across the region in how GP information is received by MES offices but in all areas their current way of working is working reasonably well.
Issues that have arisen include:
- Timeliness of referrals to the MES office: Most referrals are received promptly but there remains occasions when significant delays have been introduced by a failure of the referral from the GP surgery to reach the MES as soon as practicable after the death.
- Quality of Referral: Not accurately and completely filling out the referral form from your local MES can contribute to delays in the MES overview. If direct access by the MES to your system is not possible, you do need to send to the service sufficient information from the medical record to enable the ME to conduct a review of the care provided and review the proposed cause of death entries on the MCCD. For example, a standard EMIS summary that includes only the last three consultation entries is unlikely to be adequate.
- Completion of the MCCD: MEs ask that all parts of the MCCD are completed appropriately. You may find it helpful to refer to Guidance for Medical Practitioners completing the medical certificates of cause of death in England and Wales. It is common for the parts relating to ethnicity or the presence of implantable medical devices not to be completed appropriately which results in preventable delays for bereaved families. The ME is unable to complete these parts on your behalf.
- Form CN1A: A coroner will issue a CN1A to the attending practitioner (AP) when they have decided that their duty to investigate a death is not engaged (in other words when they are satisfied that it has been a natural death). In such circumstances, the coroner will not propose a cause of death and it will be a matter for the AP to complete the MCCD and involve the medical examiner in the usual way.
When a coroner issues a CN1A, they should also inform the medical examiner office that they have done so but there have been cases when this has not occurred.
If you receive a CN1A then you should complete the MCCD and forward it to the medical examiner office promptly (if you have any queries about the completion of the MCCD, then you could speak with the medical examiner in order to seek their advice). Please also forward to the MES office the CN1A so they are aware the Coroner has had prior involvement and has decided they do not need to investigate the death further.
Further information can be found in Guidance No 47: The Death Certification Reforms – Courts and Tribunals Judiciary.
Please do not hesitate to contact your local medical examiner office if you have any general queries about the procedures.
Which deaths require notification to the coroner?
The obligation to notify deaths to the coroner can be found in the Notification of Deaths Regulations (2019) (amended March 2020)
If the death does not fulfil the definitions as outlined in the above link, then it will amount to a non-coronial death and therefore will require medical examiner scrutiny (if you are unsure as to whether a death requires referral to the coroner, then the medical examiner will be able to advise you).
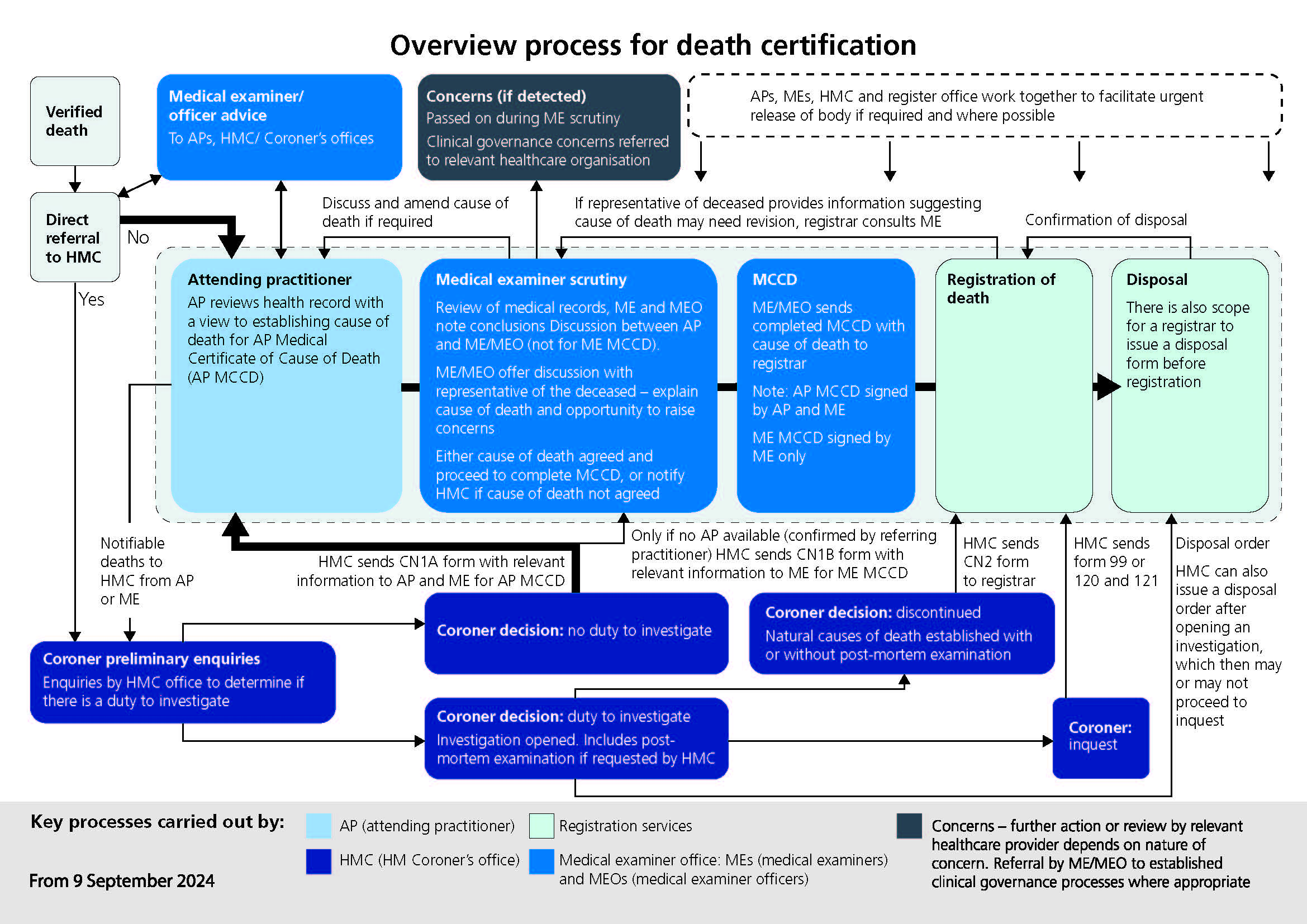
The National Medical Examiner for England and Ways has produced this flowchart explaining the new process.
Who is a medical examiner?
Medical examiners are senior medical doctors, who are trained in the legal and clinical elements of death certification processes. Their medical background can be from either primary or secondary care and most MES have a combination of both.
The role of the medical examiner includes:
- Conducting a proportionate review of the medical records.
- Liaising with the doctor who treated the patient in their final illness.
- Agreeing the proposed cause of death with the attending doctor and the overall accuracy of the medical certificate cause of death.
- Discussing the proposed cause of death with the next of kin, ensuring they understand any medical terms and providing an opportunity for them to raise any concerns, comments or compliments that they may have.
- Acting as a medical advice resource for the local coroner.
- Ensuring any concerns about the care of the patient are acted on appropriately (and if possible that any compliments are relayed to the relevant person[s]).
- Sending the completed and countersigned MCCD to the register office.
- Should they detect concerns about care, refer such cases as appropriate to established clinical governance review processes and/or notify the coroner or police when appropriate.
- Medical examiners are not responsible for verifying deaths or for confirming the identity of bodies.
Aims of the MES
The stated aims of the MES are summarised below:
- To provide greater safeguards for the public by ensuring proper scrutiny of all non-coronial deaths.
- To ensure the appropriate direction of deaths to the coroner.
- To provide a better service for the bereaved and an opportunity for them to raise any concerns to a doctor not involved in the care of the deceased.
- To improve the quality of death certification.
- To improve the quality of mortality data.
Medical examiner offices
Medical examiner offices in London are hosted by acute trusts.
The table below sets out how medical examiner offices map onto London boroughs.
| Trust/Medical examiner office | London borough(s) |
| Barking, Havering & Redbridge NHS Trust | Barking & Dagenham, Havering and Redbridge |
| Barts Health NHS Trust | City, Newham, Tower Hamlets and Waltham Forest |
| Chelsea And Westminster Hospital NHS Foundation Trust | Kensington & Chelsea and Hounslow |
| Croydon Health Services NHS Trust | Croydon |
| Epsom And St Helier University Hospitals NHS Trust | Sutton |
| Guy’s And St Thomas’ NHS Foundation Trust | Southwark and Lambeth |
| Homerton University Hospital NHS Foundation Trust | Hackney |
| Imperial College Healthcare NHS Trust | Hammersmith & Fulham and Westminster |
| Kingston Hospital NHS Foundation Trust | Kingston and Richmond |
| King’s College Hospital NHS Foundation Trust | Bromley and Bexley |
| Lewisham And Greenwich NHS Trust | Lewisham and Greenwich |
| London North West University Healthcare NHS Trust | Ealing, Brent and Harrow |
| North Middlesex University Hospital NHS Trust | Enfield and Haringey |
| Royal Free London NHS Foundation Trust | Barnet |
| St George’s University Hospitals NHS Foundation Trust | Wandsworth and Merton |
| The Hillingdon Hospitals NHS Foundation Trust | Hillingdon |
| University College London Hospitals NHS Foundation Trust | Camden |
| Whittington Health NHS Trust | Islington |
Contact details for all the Medical Examiner Offices in England a Wales can be found here.
Access to the medical records
Medical examiners have a statutory right of access to the records for the purposes of their role on the basis that they have been added to the list of persons with a right of access to patient records in the Access to Health Records Act (1990).
There is no associated funding to facilitate the provision of the records to the medical examiner. In the fulness of time, this may be resolved by medical examiners having access to the relevant records online, in the interim it is important to work with your local medical examiner office in relation to providing the relevant information that they require.
Legislation
The primary legislation that underpins the statutory MES is the Coroners and Justice Act 2009 and since its passage, the act has been amended (most recently by the Health and Care Act 2022) to reflect changes to the health system.
A summary of the changes to the legislation can be found here, however some of the key changes are as follows:
- A medical practitioner will be eligible to be an Attending Qualified Practitioner (AQP) and complete an MCCD, if they have attended the deceased in their lifetime(this removes the obligation to refer the case to a coroner for review if they had not attended the patient within the 28 days prior to death or had not seen in person the patient after death).
- The term attended has not, as yet, been defined however if a GP has made a meaningful contribution to the clinical care of the patient, this is likely to fulfil the definition. Each case will need to be judged on its merits as there may be cases when a GP’s involvement has been minimal or historic. The GP should only complete the MCCD if they feel able to propose the cause of death to the best of their knowledge and belief.
- The new MCCDs (one for the deaths of patients under the age of 28 days and one for patients over the age of 28 days) include the following additional fields:
- The details of the medical examiner who scrutinised the cause of death.
- Ethnicity, as self-declared by the patient on the medical record (if the patient medical record does not include this information, then the attending practitioner can complete it as ‘unknown’ on the MCCD and should not in any circumstance ask for this information from the representative of the deceased).
- Maternal deaths (bringing the MCCD in line with international standards).
- Medical devices and implants will be recorded on the MCCD by the attending practitioner, and this will be transferred to the certificate for burial or cremation (known as the green form) completed by the registrar in order to inform relevant authorities of the presence of any devices or implants.
- The new MCCDs will be in hard copy format, however it will be possible to scan the completed document and forward it electronically. A digital MCCD is currently in development.
Other resources
- RCGP online learning module
- The national medical examiner system (NHS England)
- NHS England medical examiner updates
- Implementing the medical examiner system – good practice guidance
- Medical examiners and general practice (informative video in which two GP medical examiners discuss their experience of the Medical Examiner System to date)
- Guidance for medical practitioners completing MCCDs in England and Wales (new version published to coincide with the implementation of the MES)
Relevant regulations: