Published 17 February 2023. Read the report in full.
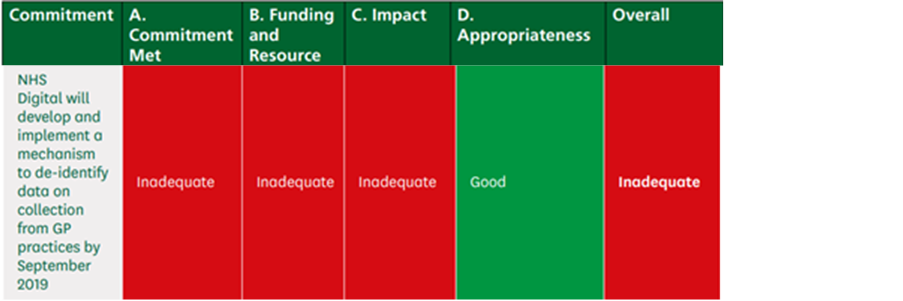
The Expert Panel identified nine commitments across four policy areas to review progress of NHS digitisation, and summarised their ratings of each in a table at the start of the report. Only one headline commitment specifically referenced GPs [pg12]:
The overall rating across all commitments is inadequate.
Sections relevant to general practice
Commitment: Our aim is that, by 2024, 75% of adults will have registered for the NHS App with 68% (over 30 million people) having done so by March 2023.
- The NHS App is not always well integrated with other systems used by GP practices, hospitals, and in community settings which can prevent use of the NHS App to manage hospital appointments and repeat prescriptions. [pg19]
- There appears to be no coherent policy nor specific funding to support the continued roll-out, which is expected to be driven primarily by GP practices without a commitment of providing them with extra financial resource to enable them to do so. [pg19]
- Some stakeholders pointed out that the roll-out of the NHS App can increase GP workload as they need to support patients to use it, or have to put alternate systems in place to ensure all patients can access their services whether or not they use the NHS App. [pg32]
- The use of multiple apps and digital systems with similar functionality within the same GP practice, as well the lack of integration between the NHS App and other systems used by GP practices, hospitals, and in community settings could make it confusing for patients who have several options to access the same digital services. [pg34]
- The 2022 GP patient survey indicated that, nationally, only 16% of patients used an online service to book a GP appointment, and this includes all websites or apps, not necessarily just the NHS App. [pg35]
- Higher numbers of registrations among GP practices in less deprived areas, as well amongst younger patients. [pg37]
Commitment: By increasing digital connection and providing more personalised care, we can support people to monitor and better manage their long-term health conditions in their own homes, enabling them to live well and independently for longer.
- We heard about a large number of individual projects using digital remote monitoring, several of which reported positive outcomes in specific groups of patients. The Department told us that home blood pressure monitoring has been rolled out via 687 GP practices volunteering as ‘trailblazers’, with early data from Dorset showing reductions in patients’ blood pressure. They also told us that 179,000 people living with diabetes have accessed home urine testing for kidney health, supported by a product that uses artificial intelligence. [pg20]
- Healthwatch referred to a study they had carried out of patients using blood pressure monitors at home, which found that nearly half of the participants were unable to submit electronic readings to their GP. [pg44]
- One GP said that with the right technology and interoperability, digital monitoring and remote care can reduce pressure on acute care and address health inequalities among patients who find it difficult to access general practice. [pg44]
Commitment: NHS Digital will develop and implement a mechanism to de-identify data on collection from GP practices by September 2019.
- The events that led to the pause of General Practice Data for Planning and Research in 2021 resulted in significant damage to public confidence and an increase in the number of patients opting out of the programme. [pg22]
- There appears to be no clear published plan, communications or consultation strategy, or timeframe for how the Government is going to address public and provider concerns, particularly around the opt-out of data sharing. Many stakeholders, including researchers and clinicians, were unclear about who will be permitted to access de-identified data, under which conditions and security Evaluation of Government commitments made on the digitisation of the NHS 23 protocols, and for which purposes. [pg22]
- Confidence among diverse communities, or evidence to re-assure providers that this will not exacerbate health inequalities.302 There is a real risk that public distrust following the withdrawal of GPDPR in 2021 will make data sharing (potentially even for direct care purposes) more contentious than it needs to be. [pg71]
- With regard to the collection of de-identified GP data for research and planning, there has been no meaningful progress in 10 years. The impact on patients of the paused GPDPR programme has so far been negative, particularly in relation to damaged trust and lost opportunities to harness patient data to improve services and conduct research. [pg71]
Commitment: Roll out of integrated care records
- Healthwatch highlighted that the implementation of new NHSE Accelerated Citizens’ Access programme (which enables patients to view their own GP medical records via the NHS App) could be affected by guidance from the BMA to GPs that they should not implement this until safe to do so. [pg56]
Commitment: “We will enable recruitment retention and growth of the digital, data, technology workforce to meet challenging projected health and care demand by 2030 through graduates, apprentices and experienced hires creating posts for an additional 10,500 full-time staff (March 2025)”
- The Practice Management Network stated that although it is possible to host graduates in GP practices and primary care settings, no funding is available to assist the practice in paying for the monitoring, development and training of the graduate. It remains unclear to us how practices will fund this, and whether it will be a priority in light of other competing budgetary demands. [pg107]
[In previous reports] We have concluded that a lack of effective workforce planning resulting in workforce shortages, and poor training, progression and staff development, can compromise patient safety and quality of care. Staff shortages coupled with increased demand means staff do not always have the capacity to undertake training on how to use digital systems and technology effectively. [pg18]

